 "I need some immediate ideas about how to deal with my son's behavior problems. He has Asperger syndrome (high functioning), ADHD and ODD. His behavior is completely out of control and I am at my wits end. Please help! He also has a lot of problems at school. His favorite thing to do when he's upset is to throw and break things."
"I need some immediate ideas about how to deal with my son's behavior problems. He has Asperger syndrome (high functioning), ADHD and ODD. His behavior is completely out of control and I am at my wits end. Please help! He also has a lot of problems at school. His favorite thing to do when he's upset is to throw and break things."
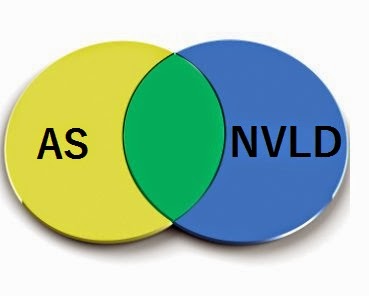
There are no easy, quick fixes to reduce or eliminate severe behavioral issues in children with Asperger’s (AS) or High-Functioning Autism (HFA) (e.g., self-injury, aggressiveness, meltdowns, tantrums, destructiveness, etc.). However, I have a few suggestions that may not require a tremendous amount of time and effort to implement. Let’s look at a few…
1. One reason for behavioral issues may be difficulties in receptive language. Kids on the autism spectrum often have poor auditory processing skills. As a result, they often don’t understand what others are saying to them; they hear the words, but they don’t understand what the words mean. The child’s lack of understanding can lead to confusion and frustration, which can escalate into a behavioral issue. Visual communication systems can be useful in teaching and in informing these children of what is planned and what is expected of them.
2. Behavioral issues may be due to difficulties in expressive language. Some researchers suggest that many behavioral issues in kids on the autism spectrum are simply due to poor expressive communication skills. There are numerous communication strategies (e.g., Picture Exchange Communication System, Simultaneous Communication), which can be used to teach expressive communication skills.
3. Food allergies can be a cause of behavior issues (e.g., dairy and wheat products, food preservatives, food coloring). Some AS and HFA children have red ears, red cheeks or dark circles under their eyes, which are often signs of food allergies. Some of the symptoms associated with food allergies include feelings of nausea, headaches, fuzzy thinking, stomach aches, meltdowns and tantrums. Due to these allergic reactions, the youngster may be less tolerant of others and more likely to act out. Since some of these “special needs” kids have poor communication skills, moms and dads may not be aware that their youngster is not feeling well. Have your son or daughter tested if food allergies are suspected.
==> How To Prevent Meltdowns and Tantrums In Children With High-Functioning Autism and Asperger's
4. In some cases, a behavior problem is a reaction to a request or demand made by the parent or educator. The AS or HFA child may have learned that he can escape or avoid certain undesirable situations (e.g., doing homework) by acting out. A functional assessment of the child’s behavior (i.e., antecedents, consequences, context of the behavior) can divulge certain relationships between the behavior and the function the behavior serves. If avoidance is the function the behavior serves, parents and educators should follow through with all requests and demands made to the child. If the child is able to escape or avoid such requests – even only some of the time – the behavior problem will continue.
5. Behavioral issues may be due to a low level of arousal (e.g., when the child is bored). Certain behaviors (e.g., aggression, destructiveness) may be exciting – and thus appealing – to the child. If it is suspected that behavioral issues are due to under-arousal, the AS or HFA child can be kept busy and active (e.g., with vigorous exercise).
6. Occasionally a youngster with AS or HFA may exhibit a behavior problem at school but not at home, or vice versa (e.g., the mom or dad may have already created a technique to stop a behavioral problem at home, but the educator is unaware of this technique). Parents and educators should discuss the youngster’s behavioral issues since one of them may have already discovered a solution to handle a particular problem.
7. Often times, powerful medications are prescribed to children on the autism spectrum to treat their behavior problems (the most common one being Ritalin). A survey conducted by the Autism Research Institute revealed that 45% of over 2,000 moms and dads felt that Ritalin made their youngster’s behavior worse.
8. Some moms and dads are giving their AS and HFA kids safe nutritional supplements (e.g., Vitamin B6 with magnesium, DMG). Nearly half have reported a reduction in behavioral issues as well as improvements in the youngster’s general well-being.
9. The AS or HFA child’s level of arousal should be considered when developing a technique to deal with behavioral issues. Sometimes “bad” behavior occurs when the child is overly-excited. This can occur when she is anxious or when there is too much stimulation in the environment. In this case, interventions should be aimed at calming the child (e.g., with vigorous exercise, vestibular stimulation, deep pressure, etc.).
==> Parenting System that Significantly Reduces Defiant Behavior in Teens with Aspergers and High-Functioning Autism
10. If the AS or HFA youngster’s behavior is worse at school but not at home, there are many possible reasons. For example:
1. One reason for behavioral issues may be difficulties in receptive language. Kids on the autism spectrum often have poor auditory processing skills. As a result, they often don’t understand what others are saying to them; they hear the words, but they don’t understand what the words mean. The child’s lack of understanding can lead to confusion and frustration, which can escalate into a behavioral issue. Visual communication systems can be useful in teaching and in informing these children of what is planned and what is expected of them.
2. Behavioral issues may be due to difficulties in expressive language. Some researchers suggest that many behavioral issues in kids on the autism spectrum are simply due to poor expressive communication skills. There are numerous communication strategies (e.g., Picture Exchange Communication System, Simultaneous Communication), which can be used to teach expressive communication skills.
3. Food allergies can be a cause of behavior issues (e.g., dairy and wheat products, food preservatives, food coloring). Some AS and HFA children have red ears, red cheeks or dark circles under their eyes, which are often signs of food allergies. Some of the symptoms associated with food allergies include feelings of nausea, headaches, fuzzy thinking, stomach aches, meltdowns and tantrums. Due to these allergic reactions, the youngster may be less tolerant of others and more likely to act out. Since some of these “special needs” kids have poor communication skills, moms and dads may not be aware that their youngster is not feeling well. Have your son or daughter tested if food allergies are suspected.
==> How To Prevent Meltdowns and Tantrums In Children With High-Functioning Autism and Asperger's
4. In some cases, a behavior problem is a reaction to a request or demand made by the parent or educator. The AS or HFA child may have learned that he can escape or avoid certain undesirable situations (e.g., doing homework) by acting out. A functional assessment of the child’s behavior (i.e., antecedents, consequences, context of the behavior) can divulge certain relationships between the behavior and the function the behavior serves. If avoidance is the function the behavior serves, parents and educators should follow through with all requests and demands made to the child. If the child is able to escape or avoid such requests – even only some of the time – the behavior problem will continue.
5. Behavioral issues may be due to a low level of arousal (e.g., when the child is bored). Certain behaviors (e.g., aggression, destructiveness) may be exciting – and thus appealing – to the child. If it is suspected that behavioral issues are due to under-arousal, the AS or HFA child can be kept busy and active (e.g., with vigorous exercise).
6. Occasionally a youngster with AS or HFA may exhibit a behavior problem at school but not at home, or vice versa (e.g., the mom or dad may have already created a technique to stop a behavioral problem at home, but the educator is unaware of this technique). Parents and educators should discuss the youngster’s behavioral issues since one of them may have already discovered a solution to handle a particular problem.
7. Often times, powerful medications are prescribed to children on the autism spectrum to treat their behavior problems (the most common one being Ritalin). A survey conducted by the Autism Research Institute revealed that 45% of over 2,000 moms and dads felt that Ritalin made their youngster’s behavior worse.
8. Some moms and dads are giving their AS and HFA kids safe nutritional supplements (e.g., Vitamin B6 with magnesium, DMG). Nearly half have reported a reduction in behavioral issues as well as improvements in the youngster’s general well-being.
9. The AS or HFA child’s level of arousal should be considered when developing a technique to deal with behavioral issues. Sometimes “bad” behavior occurs when the child is overly-excited. This can occur when she is anxious or when there is too much stimulation in the environment. In this case, interventions should be aimed at calming the child (e.g., with vigorous exercise, vestibular stimulation, deep pressure, etc.).
==> Parenting System that Significantly Reduces Defiant Behavior in Teens with Aspergers and High-Functioning Autism
10. If the AS or HFA youngster’s behavior is worse at school but not at home, there are many possible reasons. For example:
- Cleaning solvents: Custodians use powerful chemicals when cleaning the school environment. Even though the smell may be gone in a few hours, chemical residue is still in the air and on surfaces. Breathing these chemicals often affects children with sensitivities in this area. Children often place their hands and face on the tables and floors, thus cleaning solvents may end up in the youngster’s mouth and can alter brain functioning as well as behavior. Many educators who have wiped the desks with water or a natural cleaning solution prior to class each morning have reported significant improvements in their “special needs” students.
- Florescent lighting: Many kids on the autism spectrum report that florescent lights bother and distract them during classroom activities. Also, researchers have observed more repetitive, self-stimulatory behaviors under florescent lighting compared to incandescent lighting. When possible, educators may want to turn off the florescent lighting in their classroom for a few days to see if there is a decrease in behavioral issues for some of their “special needs” children. During this experiment, the educator can use natural light from the windows or incandescent lights.
- Lack of consistency, routine, or structure: Children on the autism spectrum crave structure. It helps them feel safe, and facilitates the ability to concentrate.
More resources for parents of children and teens with High-Functioning Autism and Asperger's:
==> Launching Adult Children with Asperger's and High-Functioning Autism: Guide for Parents Who Want to Promote Self-Reliance
==> Teaching Social Skills and Emotion Management to Children and Teens with Asperger's and High-Functioning Autism
==> Parenting Children and Teens with High-Functioning Autism: Comprehensive Handbook
==> Unraveling The Mystery Behind Asperger's and High-Functioning Autism: Audio Book
==> Parenting System that Reduces Problematic Behavior in Children with Asperger's and High-Functioning Autism


.jpg)


